TIM-3 therapy for Alzheimer’s is emerging as a promising approach in the realm of Alzheimer’s disease treatment, leveraging immune system checkpoint mechanisms traditionally used in cancer therapies. Recent studies have shown that inhibiting TIM-3 enables microglia, the brain’s immune cells, to effectively clear amyloid plaques, leading to notable improvements in cognitive function among treated mice. This innovative method suggests a vital link between immune response modulation and memory restoration, which opens a new frontier in addressing one of the most challenging neurodegenerative diseases. By focusing on the role of checkpoint molecules, such as TIM-3, researchers aim to restore the brain’s natural ability to combat Alzheimer’s-related damage. With the potential for significant breakthroughs in memory recovery, TIM-3 therapy could represent a paradigm shift in Alzheimer’s therapeutic strategies and innovation.
The exploration of TIM-3 as a therapeutic target for Alzheimer’s disease involves understanding the role of immune checkpoint molecules in regulating brain health. By employing strategies typically reserved for cancer treatment, scientists are delving into the possibility of enhancing microglial activity to diminish plaque build-up in the brain. This intersection of immunology and neuroscience paves the way for novel interventions aimed at cognitive function improvement in Alzheimer’s patients. With current research uncovering new pathways for addressing amyloid plaque accumulation, the application of TIM-3 therapy might redefine how we approach neurodegenerative disorders. As studies continue to evolve, the implications of this immune strategy could lead to groundbreaking advancements in the prevention and management of Alzheimer’s.
Understanding TIM-3 Therapy for Alzheimer’s Disease
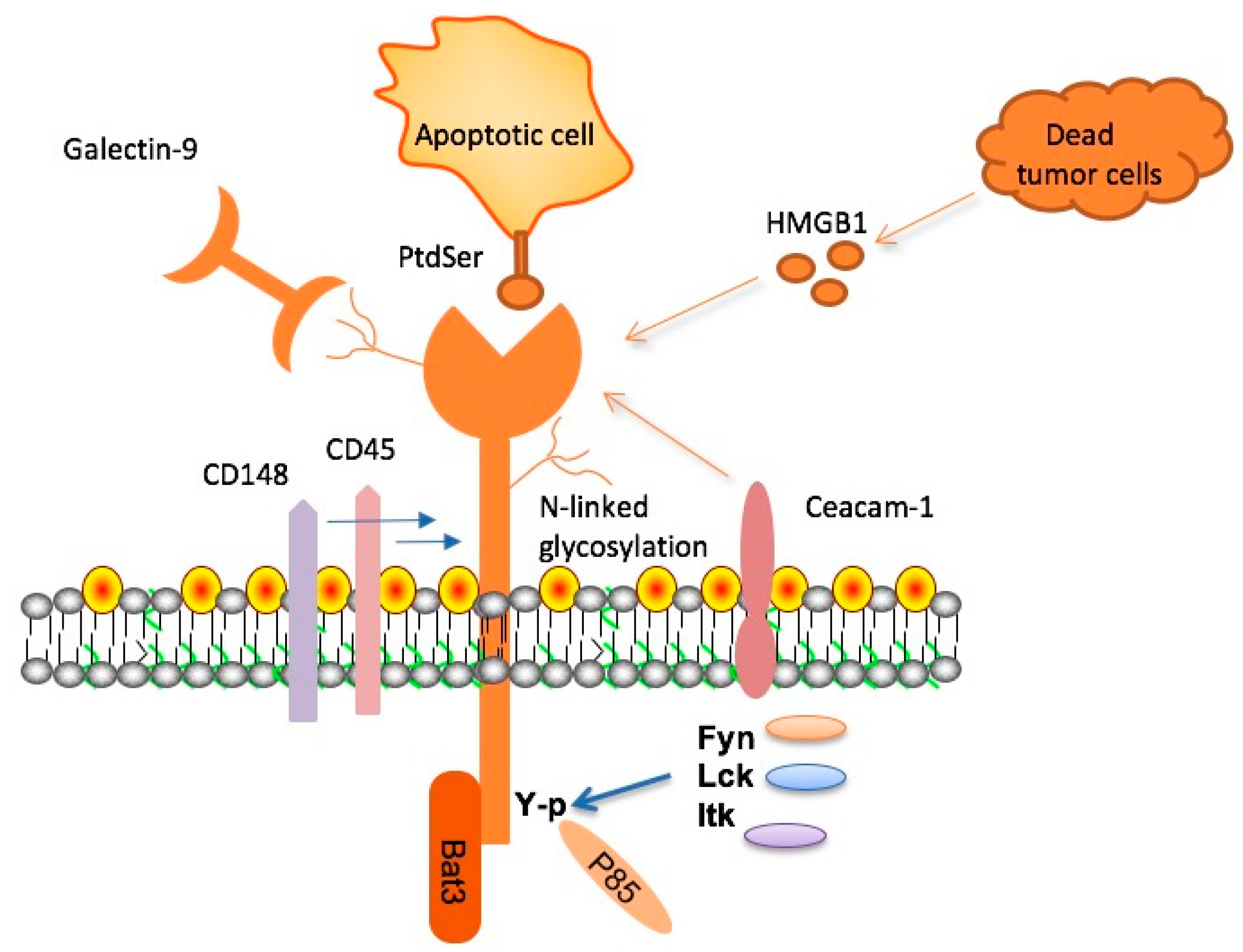
TIM-3 therapy represents a novel approach in the treatment of Alzheimer’s disease, focusing on the manipulation of immune system checkpoint molecules. TIM-3, known for its inhibitory role, has been shown to regulate the activity of microglia, the brain’s immune cells. Research indicates that the downregulation of TIM-3 can unleash these cells, enabling them to effectively combat amyloid-beta plaques in the brain. This mechanism highlights the promise of TIM-3 therapy not only in potentially slowing Alzheimer’s progression but also in improving overall cognitive function for individuals afflicted with the disease.
Current Alzheimer’s disease treatments primarily target symptoms rather than underlying mechanisms. With the advent of TIM-3 therapy, there is an opportunity to transform therapeutic strategies by harnessing the brain’s immune system. As studies have shown, inhibiting TIM-3 may reverse microglial inactivity and enhance plaque clearance, thereby tackling one of the root causes of cognitive decline. By leveraging the insights from cancer immunotherapy, this strategy could pave the way for groundbreaking advancements in Alzheimer’s disease management.
The Role of Microglia in Alzheimer’s Disease
Microglia play a crucial role in the brain’s immune response, particularly in the context of Alzheimer’s disease. These resident immune cells are responsible for clearing away debris, including amyloid-beta plaques, which accumulate and contribute to cognitive decline. However, in Alzheimer’s patients, microglia become less effective due to factors such as heightened TIM-3 expression, which inhibits their ability to phagocytose these harmful plaques. Understanding microglia’s function in Alzheimer’s is pivotal to exploring new therapies, such as TIM-3 modulation.
Research suggests that enhancing microglial function could lead to significant improvements in cognitive function for Alzheimer’s patients. By inhibiting the checkpoint molecule TIM-3, microglia can regain their ability to clear plaques and contribute positively to maintaining cognitive health. This not only underlines the importance of microglia in Alzheimer’s disease treatment but also sets a precedent for future therapies that target immune mechanisms as a means of improving cognitive outcomes.
Exploring Immune System Checkpoints in Alzheimer’s Therapy
Immune system checkpoints, like TIM-3, have been extensively studied within the context of cancer therapies, revealing their dual role in regulating immune responses. In the case of Alzheimer’s disease, these checkpoints can become detrimental, as they inhibit essential immune functions needed to manage neurodegenerative processes. The discovery that TIM-3 can restrain microglial activity might just be the key to unlocking new treatment avenues. By turning off or inhibiting these checkpoint pathways, researchers aim to enhance the brain’s immune response against amyloid plaques, which could substantially alter the progression of Alzheimer’s.
The implications of checkpoint blockade in Alzheimer’s therapy extend beyond just improving microglial function. They may also help shift the focus from symptomatic treatment to one that addresses the root causes of the disease. As researchers integrate insights from cancer therapies, there’s burgeoning interest in developing anti-TIM-3 antibodies or small molecules that could effectively target these checkpoints within the context of neurodegeneration. This innovative approach holds the potential not only for cognitive function improvement but also for a comprehensive strategy for Alzheimer’s disease treatment.
Cognitive Function Improvement through TIM-3 Inhibition
Inhibiting TIM-3 has shown promising potential to improve cognitive function in preclinical models of Alzheimer’s disease. The restoration of microglial activity leads to enhanced plaque clearance in the brain, which directly correlates with improved memory and cognitive abilities in mice. This breakthrough suggests that therapies targeting TIM-3 might reverse some of the cognitive deficits associated with Alzheimer’s, offering hope for patients currently facing frustratingly progressive symptoms.
Through rigorous testing and innovative research methodologies, scientists are exploring whether TIM-3 inhibition can yield significant results in cognitive function recovery. As cognitive decline is one of the most debilitating aspects of Alzheimer’s, the prospect of a therapy that not only addresses the accumulation of harmful plaques but also revitalizes cognitive performance is revolutionary. This approach offers a multifaceted strategy, combining immunology with cognitive neuroscience to develop seamless treatment plans for those impacted by the disease.
Repurposing Cancer Therapies for Alzheimer’s Treatment
The application of cancer therapy strategies, particularly those targeting immune checkpoints, to Alzheimer’s disease highlights an innovative crossover between oncology and neurology. The success of anti-TIM-3 antibodies in cancer has now opened new pathways to explore their therapeutic benefits for patients with Alzheimer’s. This repurposing of established cancer therapies represents a strategic pivot that might address the limitations of current Alzheimer’s treatments, particularly by enhancing the immune system’s capability to combat neurodegenerative processes.
Another exciting facet of this approach lies in the opportunity for personalized medicine in Alzheimer’s treatment. Just as cancer therapies are tailored to fit the unique genetic and epigenetic profiles of tumors, targeting TIM-3 may also be individualized based on a patient’s genetic disposition towards Alzheimer’s. This proactive strategy not only maximizes the effectiveness of existing therapies but also offers a fresh horizon in the quest to find meaningful and impactful solutions to a complex and challenging disease.
Next Steps in TIM-3 Research for Alzheimer’s Disease
As research progresses, the next steps in TIM-3 therapy for Alzheimer’s disease involve critical investigations aimed at validating findings in human models. This includes the development of transgenic mouse models that closely mimic human pathology, paving the way for the assessment of human-specific anti-TIM-3 antibodies. Continued collaboration among researchers is essential for translating these findings into clinically relevant treatments that can potentially reverse cognitive decline in Alzheimer’s patients.
Furthermore, the integration of TIM-3 research with other emerging therapies could yield a combinatory effect, enhancing overall effectiveness against Alzheimer’s. As there has been a history of failed trials in Alzheimer’s treatments, incorporating multi-faceted approaches that include TIM-3 modulation may turn the tide for successful therapeutic outcomes. Continuous funding, rigorous experimentation, and a focus on innovative treatment paradigms will be vital for making progress in this field.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s disease and how does it work?
TIM-3 therapy for Alzheimer’s disease is a novel treatment approach targeting the TIM-3 checkpoint molecule in the brain. This therapy aims to enhance the activity of microglia, the immune cells responsible for clearing amyloid plaques associated with Alzheimer’s. By inhibiting TIM-3, microglia are freed to attack these plaques, potentially improving cognitive function and memory.
How does TIM-3 impact microglia and Alzheimer’s treatment?
TIM-3 is an immune system checkpoint that, when overexpressed in microglia, prevents these cells from clearing amyloid plaques in the brains of Alzheimer’s patients. By developing TIM-3 therapy, researchers aim to inhibit this checkpoint, allowing microglia to regain their function and thus play a crucial role in Alzheimer’s disease treatment by clearing toxic plaques.
What role does TIM-3 play in the immune response related to Alzheimer’s disease?
In the context of Alzheimer’s disease, TIM-3 acts as an inhibitory checkpoint for microglia, which are the brain’s immune cells. When TIM-3 levels are high, microglia become less effective at targeting and clearing amyloid beta plaques, leading to increased plaque accumulation. TIM-3 therapy seeks to deactivate this inhibition, enhancing the immune response in Alzheimer’s treatment.
Can TIM-3 therapy improve cognitive function in Alzheimer’s patients?
Yes, TIM-3 therapy has shown promise in preclinical models. By inhibiting the TIM-3 checkpoint, researchers have observed that microglia can effectively clear plaques, which is associated with cognitive function improvement. While ongoing studies continue to assess its effectiveness in humans, initial results are encouraging.
What types of interventions are being explored in TIM-3 therapy for Alzheimer’s?
Interventions in TIM-3 therapy for Alzheimer’s include using anti-TIM-3 antibodies and small molecules designed to inhibit the functions of TIM-3. These approaches aim to enhance microglial activity and plaque clearance in the brain, potentially leading to effective Alzheimer’s disease treatments.
Is TIM-3 therapy similar to immune checkpoint therapies used in cancer treatment?
Yes, TIM-3 therapy for Alzheimer’s shares principles with immune checkpoint therapies in cancer treatment. Both strategies involve targeting checkpoint molecules to enhance immune responses. In cancer therapy, this allows T cells to attack tumors, while in Alzheimer’s, it enables microglia to clear harmful plaques.
What is the significance of the research on TIM-3 and Alzheimer’s disease?
The research on TIM-3 and Alzheimer’s disease is significant as it provides a potential new avenue for treatment based on immunotherapy principles. By focusing on the TIM-3 checkpoint, scientists hope to develop effective strategies to combat plaque accumulation, a key factor in Alzheimer’s pathogenesis, thus enhancing treatment possibilities.
What are the long-term goals of TIM-3 research in Alzheimer’s therapy?
The long-term goals of TIM-3 research in Alzheimer’s therapy include validating the efficacy of TIM-3 inhibitors in human clinical trials, understanding the mechanism of TIM-3 in Alzheimer’s progression, and ultimately providing a safe and effective treatment to improve cognitive function in Alzheimer’s patients.
What are the challenges faced in developing TIM-3 therapy for Alzheimer’s disease?
Challenges in developing TIM-3 therapy for Alzheimer’s include ensuring the treatment selectively targets plaques without affecting crucial brain functions, overcoming potential side effects, and effectively delivering therapies across the blood-brain barrier. Ongoing research aims to address these challenges to develop a viable treatment.
| Key Points |
|---|
| TIM-3 therapy may offer a new strategy for treating Alzheimer’s by overcoming the inhibition of microglia that prevents plaque clearance. |
| The study demonstrates that inhibiting TIM-3 allows microglia to attack and clear amyloid plaques, improving cognitive function in mice. |
| Late-onset Alzheimer’s represents 90-95% of all cases, and TIM-3 is linked to this form of the disease as a genetic risk factor. |
| Microglia, the brain’s immune cells, play a crucial role in removing debris but are hindered by TIM-3 in Alzheimer’s patients. |
| The research also involved genetically modifying mice to lack the TIM-3 gene, leading to improved cognitive behavior by enhancing plaque clearance. |
| Next steps include testing human anti-TIM-3 antibodies in mouse models to see if they can help prevent plaque build-up in Alzheimer’s. |
Summary
TIM-3 therapy for Alzheimer’s is emerging as a promising approach to enhance cognitive function and address the challenges posed by amyloid plaque accumulation in the brain. As research progresses, it is crucial to explore how inhibiting the TIM-3 molecule can restore the activity of microglia, potentially leading to significant breakthroughs in Alzheimer’s treatment.