Microglial Research: A Breakthrough Against Alzheimer’s Disease

Microglial research is increasingly vital in our understanding of neurodegenerative disorders, particularly Alzheimer’s disease. As the primary immune cells in the brain, microglia play a crucial role in maintaining neural health through processes like synaptic pruning, where they remove unnecessary synapses to optimize communication among neurons. However, recent studies led by renowned neuroscientist Beth Stevens show that malfunctioning microglia can contribute to the progression of Alzheimer’s and similar diseases, highlighting their complex dual role in brain function and pathology. With over 7 million Americans affected by Alzheimer’s, insights from microglial research could lead to groundbreaking biomarkers and therapies to combat these debilitating conditions. As we delve deeper into the brain’s immune system, we uncover how the intricate balance maintained by microglia could be pivotal in developing future treatments for neurodegenerative disorders.
Exploring the realm of brain immunology, research focused on glial cells, particularly the microglia, is at the forefront of addressing neurological diseases like Alzheimer’s. These specialized cells are integral to the brain’s defense mechanisms, facilitating the clearance of debris and refining neural circuitry through synaptic remodeling. Investigative efforts into the behavior of these brain-resident immune entities, including significant contributions from scientists like Beth Stevens, illuminate their role in both protective and pathological processes associated with cognitive decline. The ongoing research aims to pinpoint how dysregulated microglial activity can precipitate neurodegenerative disease onset and progression, ultimately striving to design novel therapeutic strategies. By understanding the delicate interplay between microglia and neuronal health, we may pave the way for innovative approaches in managing and treating widespread neurodegenerative ailments.
Understanding Microglial Cells: The Brain’s Immune System
Microglial cells are crucial components of the brain’s immune system, acting as the first line of defense against any form of injury or illness. These cells constantly patrol the brain’s intricate environment, searching for signs of damage, infection, or neural debris. Once they detect any abnormality, microglia engage in a process known as synaptic pruning, where they remove unwanted synapses. This is essential for maintaining the brain’s health and function. However, when these cells misbehave, they can disrupt normal synaptic pruning, leading to significant neurodegenerative issues, including Alzheimer’s disease.
Research spearheaded by Beth Stevens at Boston Children’s Hospital has highlighted the dual nature of microglial function. While they play a vital role in neural homeostasis, aberrant behavior can exacerbate conditions like Alzheimer’s and Huntington’s disease. Stevens emphasizes that understanding microglial cells is not just about studying their physiological roles but also about unraveling their intricate relationship with neurodegenerative disorders. By investigating microglial research, scientists are uncovering potential biomarkers that could revolutionize our approach to diagnosing and treating these conditions.
The Role of Synaptic Pruning in Neurodegenerative Disorders
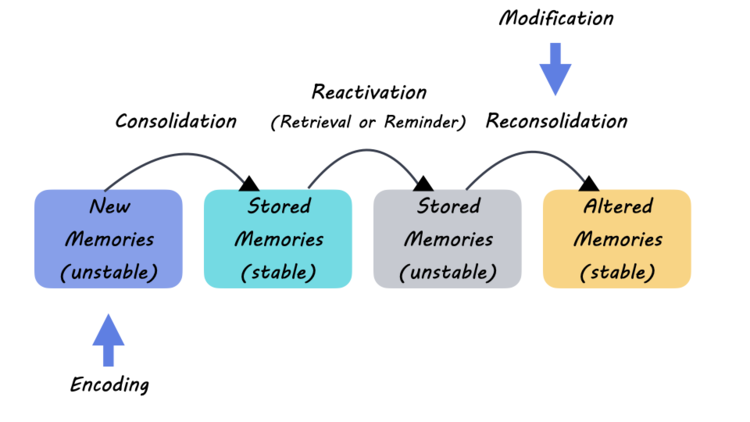
Synaptic pruning is a critical developmental process where extra synapses are eliminated, enabling more efficient neural circuits. This process is primarily performed by microglia and is vital during early life in shaping the brain’s structure and function. However, in disorders such as Alzheimer’s disease, this pruning process can become detrimental. Abnormal synaptic pruning leads to excessive synapse loss, ultimately impairing cognitive functions. Understanding the mechanisms that regulate synaptic pruning offers insights into Alzheimer’s pathology and presents pathways for potential therapeutic interventions.
Beth Stevens’ pioneering work sheds light on how dysregulated synaptic pruning can accelerate the progression of neurodegenerative disorders. By simulating various conditions and observing microglial activity, her research reveals the complexity of this immune response in the brain. The findings indicate that preventive strategies targeting synaptic pruning could hold the key to slowing down or even reversing the damage caused by diseases like Alzheimer’s. As the field of neuroscience evolves, the interplay between microglial activity and synaptic maintenance will undoubtedly be crucial in developing effective treatments.
Alzheimer’s Disease and Microglial Dysfunction
Alzheimer’s disease remains one of the most perplexing neurodegenerative disorders, characterized by cognitive decline, memory loss, and significant brain atrophy. Recent research suggests that dysfunction in microglial cells might be a significant contributor to the disease’s progression. Stevens’ studies emphasize that when microglia fail to properly prune synapses or clear out neuronal debris, toxic proteins such as amyloid-beta accumulate, forming plaques that signify Alzheimer’s.
Given the pivotal role of microglial dysfunction in Alzheimer’s pathology, understanding these cells could lead to groundbreaking therapeutic strategies. By focusing on microglial behavior, researchers aim to identify biomarkers that reflect disease progression and response to treatment. This approach aligns with a broader understanding of the interplay between the brain’s immune system and neurodegenerative diseases, highlighting how targeted interventions on microglial functions could provide relief and improve outcomes for millions of affected individuals.
Beth Stevens: A Pioneer in Neuroimmunology
Beth Stevens has emerged as a leading figure in the realm of neuroimmunology, specifically in exploring the functions of microglial cells in health and disease. Her groundbreaking research has shifted perceptions about the brain’s immune system, revealing its critical role in maintaining synaptic integrity and overall brain health. By meticulously studying microglia, Stevens has been able to connect the dots between immune response and neurodegenerative diseases, providing new avenues for research and potential therapeutic targets.
Stevens’ recognition as a MacArthur ‘genius’ is a testament to her innovative contributions, which have paved the way for new understandings of how the brain operates under both normal and pathological conditions. Her work continues to inspire a new generation of neuroscientists who are exploring the untapped potential of the brain’s immune system. By investigating microglial behavior, she emphasizes that fundamental research is crucial for translating discoveries into practices that could benefit patients suffering from Alzheimer’s and other related disorders.
Federal Funding and Its Impact on Alzheimer’s Research
Federal funding plays a significant role in advancing critical research into Alzheimer’s disease and other neurodegenerative disorders. Beth Stevens notes that her foundational research was significantly supported by grants from the National Institutes of Health (NIH) and other federal agencies. This financial backing allows scientists to explore complex biological systems like microglia without the immediate pressure of producing commercially viable results, thereby fueling innovation and discovery.
Such funding is essential, especially in a field that delves into the intricate workings of the brain. It enables researchers to pursue basic and curiosity-driven science, laying the groundwork for future breakthroughs in treating Alzheimer’s and related neurodegenerative disorders. As Stevens aptly illustrates, sometimes the most profound insights come from seemingly unrelated studies, reiterating the need for continued investment in scientific exploration to tackle diseases that currently have no cure.
Emerging Biomarkers in Neurodegenerative Disease Research
The identification of biomarkers is a front-runner in the realm of Alzheimer’s research, with the potential to revolutionize how we understand and treat this complex disorder. Biomarkers serve as biological indicators of disease states, enabling earlier diagnosis, monitoring progression, and assessing responses to therapy. Beth Stevens’s research on microglial behavior has laid the foundation for discovering novel biomarkers associated with neurodegenerative processes, particularly those influenced by aberrant synaptic pruning.
By decoding the signaling pathways within microglial cells, researchers are uncovering biological markers that could predict the onset of Alzheimer’s disease long before clinical symptoms manifest. This proactive approach is crucial for developing effective treatments and improving patient outcomes. As the science of biomarkers continues to evolve, the insights gained from microglial research will undoubtedly play a central role in enhancing our understanding and management of neurodegenerative diseases.
Strategies for Supporting Brain Health
Maintaining brain health is essential for reducing the risk of neurodegenerative disorders like Alzheimer’s disease. Various strategies can promote optimal microglial function and overall brain wellness. Regular physical activity, a balanced diet rich in antioxidants, and engaging in cognitive exercises are fundamental ways to support neural health. Researchers, including Stevens, are increasingly interested in how lifestyle factors influence microglial activity and health, emphasizing the importance of a holistic approach to brain wellness.
Additionally, emerging evidence suggests that social interaction and mental engagement play crucial roles in maintaining cognitive function as we age. By fostering an environment that encourages both physical and mental challenges, individuals can potentially mitigate the risk of neurodegenerative diseases. As our understanding of the brain’s immune system and microglial function expands, integrating these lifestyle approaches could form a comprehensive strategy for enhancing brain health and longevity.
Future Directions in Neuroimmune Research
As the study of the brain’s immune system continues to advance, future research will undoubtedly unveil novel insights into microglial function and their implications for neurodegenerative disorders. The integration of cutting-edge technologies, such as single-cell RNA sequencing and advanced imaging techniques, allows scientists to explore microglial behavior on a cellular level. This level of granularity can lead to breakthroughs in understanding how these cells contribute to various neurodegenerative conditions, including Alzheimer’s disease.
Moreover, interdisciplinary collaborations between neuroscientists, immunologists, and geneticists are crucial for unraveling the complex interactions between the brain’s immune system and neuronal health. As exemplified by Stevens’ approach, these collaborative efforts could foster innovative therapeutic strategies that not only address the symptoms of Alzheimer’s but also tackle the underlying pathophysiological mechanisms driven by microglial dysfunction. The future of neuroimmune research promises exciting developments that could revolutionize our understanding of brain health and disease management.
Frequently Asked Questions
What is the role of microglial research in understanding Alzheimer’s disease?
Microglial research plays a crucial role in understanding Alzheimer’s disease as it investigates how microglial cells, which are the brain’s immune system, interact with neuronal health. These cells perform vital functions such as clearing dead neurons and pruned synapses, which, when functioning abnormally, can contribute to neurodegenerative disorders like Alzheimer’s.
How do microglial cells affect synaptic pruning in neurodegenerative disorders?
Microglial cells are essential for synaptic pruning, a process that refines neuronal connections during development. In neurodegenerative disorders, including Alzheimer’s disease, aberrant synaptic pruning by faulty microglial activity can lead to the loss of critical neuronal connections, exacerbating cognitive decline.
What findings has Beth Stevens contributed to microglial research?
Beth Stevens has significantly advanced microglial research by revealing how these brain immune cells can inadvertently contribute to Alzheimer’s disease through aberrant pruning of synapses. Her work has helped to establish foundational knowledge for developing new biomarkers and therapies for neurodegenerative disorders.
Can microglial research lead to new treatments for Alzheimer’s disease?
Yes, microglial research could lead to new treatments for Alzheimer’s disease. By understanding how microglial cells contribute to synaptic pruning and neuroinflammation in Alzheimer’s, scientists can identify potential targets for therapies that may improve outcomes for patients suffering from this incurable condition.
What is the significance of studying microglia in the context of neurodegenerative disorders?
Studying microglia is significant in neurodegenerative disorders because these cells are integral to the brain’s immune response. Their role in synaptic pruning and inflammation can reveal underlying mechanisms of diseases like Alzheimer’s, potentially leading to breakthroughs in treatment and patient care.
How has federal funding influenced microglial research led by Beth Stevens?
Federal funding, notably from the National Institutes of Health, has been pivotal in supporting Beth Stevens’ microglial research. This support has allowed for extensive exploration of how microglia interact with neurodegenerative diseases, advancing our understanding of conditions like Alzheimer’s.
What potential do microglial biomarkers have in Alzheimer’s disease research?
Microglial biomarkers hold great potential in Alzheimer’s disease research as they can help detect changes in microglial function that precede clinical symptoms of the disease. This could facilitate early diagnosis and the development of targeted therapies that mitigate neurodegeneration.
Why is basic science important for the future of microglial research?
Basic science is crucial for microglial research because it lays the groundwork for understanding complex biological processes. Innovations in microglial function identified through basic studies can lead to unexpected discoveries and therapeutic strategies for Alzheimer’s and other neurodegenerative disorders.
| Key Point | Details |
|---|---|
| Role of Microglial Cells | Microglia act as the brain’s immune system, clearing dead or damaged cells and pruning synapses. |
| Implications for Alzheimer’s Disease | Aberrant pruning by microglia contributes to disorders like Alzheimer’s and Huntington’s. |
| Research Funding | Stevens’ research has been largely supported by NIH funding, demonstrating the importance of federal support in scientific discovery. |
| Basic Science and Disease Connection | Basic research can seem distant from disease implications, but it plays a crucial role in understanding and developing treatments for human diseases. |
| Future of Microglial Research | The ongoing research into microglia has potential applications for developing new biomarkers and medications for neurodegenerative diseases. |
Summary
Microglial research is revolutionizing our understanding of brain health and disease. This vital work conducted by Beth Stevens and her team showcases the crucial role that microglial cells play in maintaining brain homeostasis and how their dysfunction contributes to severe neurodegenerative disorders like Alzheimer’s disease. As researchers continue to explore the complexities of microglial function and its implications in disease, they pave the way for potential breakthroughs in the diagnosis and treatment of conditions affecting millions, underscoring the importance of continued support for basic scientific research.